In addition, DMPM has been reported following radiation therapy, mica exposure, recurrent peritonitis, and administration of thorium dioxide.9–13
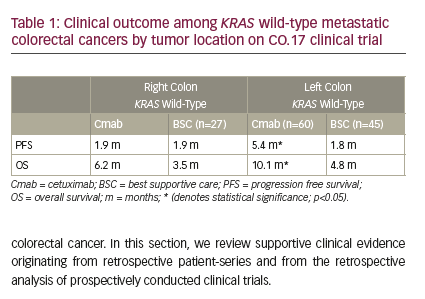
A great majority of patients present with abdominal pain and distension caused by the accumulation of tumors and ascitic fluid.14Without aggressive treatments the disease is rapidly fatal.15 In the past, DMPM was treated at most cancer centers with a combination of systemic chemotherapy, palliative surgery, and, in a few patients, total abdominal radiation. However, the patients did not seem to respond to these treatments in that the median survival was approximately one year (see Table 1).16–22 No randomized trials have been attempted but it is likely that the survival associated with these palliative treatments was little different from the natural course of the disease.
In most patients DMPM remains localized within the abdominopelvic cavity throughout its course. An aggressive treatment plan to surgically eradicate gross disease combined with peri-operative intraperitoneal chemotherapy (PIC) to control residual disease has a strong locoregional treatment rationale.23–25 This combined modality has been used with success in patients with pseudomyxoma peritonei and peritoneal carcinomatosis from other gastrointestinal and gynecologic malignancies.26–31 Treatment of peritoneal carcinomatosis through the use of intraperitoneal chemotherapy was declared standard of practice by the National Cancer Institute, Bethesda, US after a recent phase III study in ovarian cancer.32 Especially in the last five years, as the cytoreductive surgical (CRS) approach combined with PIC was expanded, the results of treatment for DMPM have dramatically improved compared with historical controls.The median survival has approached five years.14,33–49 Assessment of Survival
The effectiveness of CRS and PIC on survival of patients with DMPM is demonstrated in Table 2.39,42,45,47–49 The median survival ranged from 34 to 92 months.39,42,47,48 The median survival was not reached in two of the studies.45,49 The one-, two-, three-, five- and seven-year survival rates varied from 60% to 88%, 60% to 77%, 43% to 65%, 29% to 59%, and 33% to 39%, respectively.39,42,45,47–49 One study reported disease status in 49 patients, which showed that 29 patients had no evidence of disease; 10 patients were alive with disease; and 10 patients had died from disease.45
Assessment of Peri-operative Outcomes
The effectiveness of CRS and PIC on peri-operative outcomes is demonstrated in Table 3.38,42,45,47–49 The overall morbidity rate varied from 25% to 40%.38,39,42,45,47,49 Hematological toxicity rate varied from 8% to 26%.38,42 Blood loss was reported to be 590.38 Mean operative duration ranged from 6.5 hours to 9.6 hours.38,42,49 Reoperation rates for post-operative adverse events were 4–11%.38,42,49 The overall mortality rates ranged from 0% to 8%.38,42,45,47–49 The median and mean hospital stay were 16 days 47 and 22–23 days,38,49 respectively.
NA = median survival was not reached.
Discussion
DMPM represents one-third of all mesotheliomas and in the past attracted little attention.2-3 Traditionally there was a historic agreement among practitioners that peritoneal malignancy was virtually untreatable and therefore considered a pre-terminal condition. The patients were managed with systemic chemotherapy and palliative surgery. However, eventually nearly all patients died from the disease as a result of intestinal obstruction and/or terminal starvation.16–22 As shown in Table 1, the median survival in these patients prior to the year 2000 was less than one year. Recently, as shown in Table 2, there has been a re-examination of the peritoneal malignancy and its treatments involving CRS and PIC with a curative intent.
CRS is an important first step in the combined treatment that attempts a removal of all peritoneal tumors together with complete lysis of adhesions between the bowel loops.23 This provides an optimal situation for adjuvant intra-peritoneal chemotherapy, which is given before the formation of any adhesions, allowing direct chemotherapy and tumor-cell contact, minimizing systemic toxicity.24-25 Hyperthermia has been known to have direct cytotoxic effects in both a temperature- and time-dependent manner.50-51 It also has been shown that a greater depth of penetration of the chemotherapy agents into the tumors is achieved;52 in addition, heat synergizes the cytotoxic drugs selected for intraperitoneal use at the time of surgery.53 Many unanswered questions remain regarding the surgical options in the management of DMPM.What can be stated with assurance is that this disease, which in the past was considered a pre-terminal condition, can now be treated with CRS and PIC with benefit in terms of long-term survival. Perhaps it is safe to suggest that this new treatment option, using combined therapy, is a new standard of care with which all other treatment options should now be compared.54 However, it is also important to note that the results achieved by international experts in this field may not be replicated in routine clinical practice. In the current literature, unfortunately, there are limited data, but with increased recognition of this new treatment for DMPM, more clinical evidence will be available.