In recent years, personalized therapies have transformed the management of many advanced malignancies. However, despite advances in targeted therapy and immunotherapy that have expanded the treatment options for patients with metastatic kidney cancer, we are unable to predict which patients are most likely to respond to individual treatments.1 With a number of highly effective therapies available, it is becoming increasingly important to develop a more tailored approach to treatment selection.
In an expert interview, conducted at the American Society of Clinical Oncology (ASCO) Annual Meeting, which was held from June 1–5, 2018 in Chicago, Illinois, Ulka Vaishampayan discusses the role of personalized therapy in patients with advanced renal cancer and the potential role of X4P-001 in treatment paradigms in the future.
Q. What are the main unmet needs in the treatment of advanced renal cancer?
In the last few years a number of new treatments have emerged for advanced renal cancer but none have been compared head-to-head. Another problem is that we do not have good predictive markers to inform our therapeutic choices.
Q. What factors do you take into account when selecting a therapy for an individual patient with advanced renal cancer?
The two major criteria are the patient characteristics and the tumor characteristics. I consider the performance status of the patient, their age, and comorbidities, as well as the findings of laboratory tests such as lactate dehydrogenase (LDH), calcium, and blood counts, particularly neutrophils and platelets. Also of importance are the clinical symptoms of the patient and the interval from their first diagnosis to when they present with metastatic disease. Tumor characteristics include the location of metastases – predominantly brain or bone – or areas where they are likely to bleed or cause compression, which would result in the onset of symptoms fairly quickly.
Q. What are the most useful molecular markers to inform selection of therapy?
Currently there are no validated molecular biomarkers to help us in our therapeutic choices in renal cancer. However, a number of biomarkers are very interesting and showing promising results. The most important is programmed death-ligand 1 (PD-L1). PD-L1 positivity tells us that the patient is more likely to respond to immunotherapy, although, although patients with PD-L1-negative tumors have also benefitted from immunotherapy.2 The other interesting markers that are being researched are BAP1 mutations and PBRM1 mutations.3 These have shown the potential to predict response to immunotherapy, or lack thereof.4 Other possible markers are easily accessible, such as neutrophil/lymphocyte ratio,5 and the time of response on previous anti-vascular endothelial growth factor (VEGF) therapy. This can be useful when considering immunotherapy in the second-line setting because there is a type of kidney cancer that is likely to be more responsive to the anti-VEGF pathway than to immunotherapy.
Q. What is the mechanism of action of X4P-001?
X4P-001 is an inhibitor of the chemokine receptor CXCR4. CXCR4 overexpression has been shown to play a role in the progression of renal cancer metastases as well as being found in brain metastases.
Q. Could you tell us a little about your recent phase I/II study evaluating the efficacy and safety of X4P-001 in combination with axitinib?
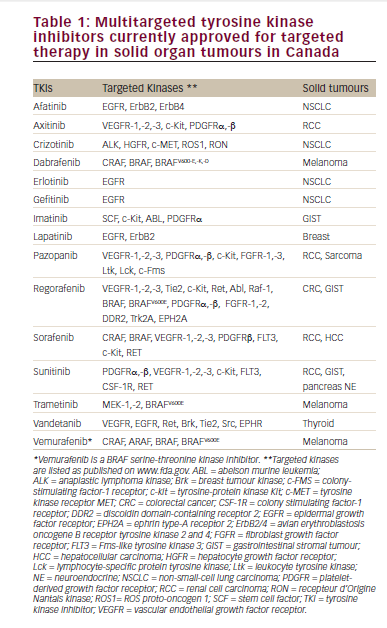
In kidney cancer there is an unmet need for new therapies as not all patients respond to, or experience, remission with currently available therapies. The addition of X4P-001 to tyrosine kinase inhibitors (TKIs), such as axitinib, increases the efficacy and delays the onset of TKI resistance.6 X4P-001 was therefore developed for kidney cancer in combination with axitinib as a third-line therapy following immunotherapy as well as failure of anti-VEGF therapies. This study enrolled patients with advanced clear cell renal cell carcinoma who had failed at least one prior therapy. Results showed that the combination is tolerable and established the optimum dosage. In addition, the efficacy findings were promising in terms of response rates and duration of response, exceeding 6–12 months.